Legg-Calvé-Perthes disease (LCPD) is a rare but serious orthopaedic condition that affects the hip joint in dogs, particularly small and toy breeds. This article will provide a comprehensive overview of LCPD, discussing its causes, symptoms, diagnosis, treatment, and prognosis.
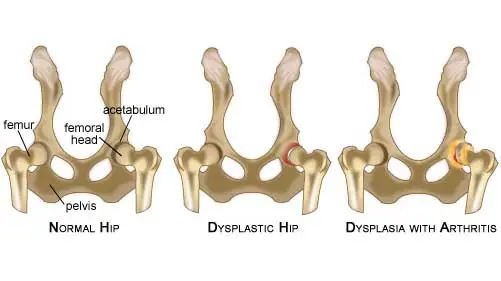
LCPD is a degenerative bone condition that primarily affects the ball-shaped end of the femur, known as the femoral head. It involves a disruption of blood flow to the femoral head, causing the bone to weaken, break down, and eventually collapse. This can lead to inflammation, pain, and degeneration of the hip joint.


The exact cause of LCPD is still unknown. However, it is believed to be a result of genetic and environmental factors. Some of the risk factors associated with the disease include:

The symptoms of LCPD can vary depending on the severity of the condition. Common signs include:
A veterinarian will conduct a thorough physical examination and take a detailed history of your dog’s health. They may perform specific joint manipulation tests to assess the range of motion and pain in the hip joint. To confirm the diagnosis, the veterinarian will likely recommend X-rays of the affected hip joint. This imaging will reveal characteristic changes in the femoral head, such as fragmentation, flattening, or collapse.
The treatment for LCPD depends on the severity of the disease and the individual dog. Non-surgical treatment options may be recommended for mild cases, which can include:
In more severe cases, surgery may be necessary to restore function to the hip joint. The most common surgical procedure is femoral head and neck ostectomy (FHO), which involves removing the damaged femoral head and neck. This allows the formation of a “false” joint, alleviating pain and improving mobility.

This older technique was popular in the 1970s. It involves cutting the pectinious muscle of the groin to lessen the pain of dysplasia. Cutting this muscle was said to decrease the normal pressure that presses the ball of the femur into the acetabular socket. Some veterinarians thought it might be helpful in certain cases of hip dysplasia. However, the relief provided was usually temporary and arthritic changes in the joint continued or possibly sped up. Few veterinarians still perform this surgery but it is no longer recommended by most veterinarians.
If the Hip Dysplasia in your pet is not severe yet, it does not mean that you should not do anything. Early diagnosis allows pet owner to prepare and possibly prevent it from getting worst. Or if surgery is not an option, there are more natural ways to management and live with a dog diagnosed with hip dysplasia.
Triple Pelvic Osteotomy procedure has been used since the early 1990s. It works best when hip dysplasia is discovered very early – before degenerative changes and arthritis become noticeable on radiographs. Dogs need to be 7 – 8 month old or older to have this surgery and it generally does not yield good results when dogs are over 12 months old. The bones that form the hip are not mature enough to hold the screws and plates that are used when the puppy is too young. And the pet will not have the full potential to remodel the new joint structure if it has finished most of its growth. So the window or time when the surgery is most effective is quite small.
It is also very difficult to perform this surgery on dogs that weigh less than 45 pounds because the surgeon must work in such a tight space.
This surgery entails cutting free the socket or acetabulum at three points (A,B&C) and rotating it so that the pressure of the femoral head is directly into the cup and not pressing on it’s upper edge. Metal plates, screws and wire are used to reattach the acetabulum to the pelvis in its new position. Recovery from the operation, which is performed only on one leg at a time, is 6-10 weeks. Surgeons that perform this operation are quite enthusiastic about the results they obtain. However, “Results suggest that JPS and TPO have similar effects on hip joint conformation in dogs with moderate to severe hip dysplasia but that neither procedure eliminates the hip joint laxity characteristic of hip dysplasia or the progression of the degenerative joint changes. If you are considering this surgery for your pet, ask the prospective surgeon to discuss these 2007 University of Wisconsin results.
During Femoral Head Osteotomy surgery, the head and neck of the femur are removed. After that is done, a flexible , fibrous attachment (pseudo-joint) naturally forms between the end of the femur and the pelvis. This should allow pain-free experience use of your pet’s leg.
The surgery is straightforward. The results are usually excellent when the dog’s adult weight is 45 pounds or less. It does not work well for heavier dogs. It can take up to a year for full motion and weight-bearing to return. But it is a real joy to see these pets racing happily and pain-free once again. When hip dysplasia affects both legs, operating on both hips simultaneously is preferred. This forces the dog to use both rear legs soon after the operation and prevents them from just carrying the repaired leg.
In hip dysplasia, it is the friction and grinding of the head of the femur against the socket of the pelvis that causes the pain. When the head of the femur is removed, the surgeon places muscular and connective tissue between the two former joint surfaces. As this consolidates with additional new scar and cartilaginous tissue, this pseudo-joint becomes pain free and allows almost natural motion. The pet will maintain the knee on that leg slightly straighter to compensate for the slight shortening of the femur.
For the first few weeks after surgery, many veterinarians confine the pet to a small cage and have the owner frequently massage the muscles of the leg. By the fourth to sixth week after surgery, your veterinarian may encourage as much light activity as possible to prevent further atrophy (withering) of the muscles of the leg. Many have the owners passively flex and extend the leg and continue massages four times a day. Dogs and cats do quite well on three legs so it is difficult to get them to start using the repaired leg. Sometimes I resort to taping a sock onto their good rear leg to encourage them to use the newly reconstructed joint. It is also proven that swimming really hastens recovery and use of the affected leg.
Within six months of surgery almost all dogs run about as if nothing had happened.
A total artificial hip replacement or prosthetic joint is also an option for your pet. It replaces the painful arthritic joint and can be performed at any stage of the disease. This process has become routine in humans but cost limits its use in dogs. It is the only technique that works in dogs over fifty pounds with advanced dysplasia. The modular prosthetic hip replacement system used today has three components, a femoral stem, a femoral head, and the artificial acetabulum. Each component has many available sizes, which allow for a custom fit. The components are made of cobalt chrome stainless steel or titanium and ultra high molecular weight polyethylene or another advanced self-lubricating plastic.
This procedure is quite expensive and only performed at large veterinary centers. It has a high success rate and changes in the dog’s mobility are nothing short of miraculous.
The surgery can be performed on dogs of any weight and at any adult age – as long as their general health is good. It’s biggest disadvantage is its cost. Hips are usually replaced one at a time. Often, one replaced hip is enough to restore the pet’s mobility.
The technique for total hip replacement in dogs was pioneered by veterinary surgeons at Ohio State University. Their orthopedic group still performs more canine hip replacements than any other university or private practice in the World.

Weight control is an important aspect of recovery and is recommended to decrease the pressure applied to the painful joint as the dog moves. You and your veterinarian will need to work together to minimize any weight gain associated with reduced exercise during recovery. Special diets designed for rapidly growing large-breed dogs may decrease the severity of hip dysplasia
Arthritis arising from hip dysplasia is commonly known as secondary Osteoarthritis it is important to correct this condition as soon as it is recognized in order to delay the development of degenerative joint disease. If surgical correction is not an option, medical management of degenerative joint disease must include gentle and controlled exercise, weight management, nutritional support and medications to control pain and discomfort.

It has been found that puppies that reach their final mature body weight a bit later in life do not develop the degree of hip dysplasia found in puppies that are allowed to eat as much as they will. The secret is to keep the puppies growing steadily but to feed them approximately twenty percent less than they would consume when fed free choice.

There will come a time when it becomes too painful for your pet to climb stairs or go outside to relieve itself. Building a handicap ramp can be helpful and some pets can be paper trained. You will think of other ways you can make life easier for pets with advanced hip dysplasia, that includes lowering some of your furniture and placing rubber non-slip mats in your house.
When you take your pet for walks and exercise, try to stay on unpaved grassy areas that cushion his step. Avoid hard packed pavement and concrete surfaces. This will lessen shock-trauma to his hips as he walks or runs. And the worst thing for a dog with hip dysplasia is sleeping on a cold, hard floor. Wood floors and carpets improve matters, but the dog will be most comfortable with an overstuffed dog bed or something similar. Orthopedic foam is also excellent.

Physical therapy can go a long way in reducing your pet’s pain and debility when dealing with hip dysplasia. Hire a professional or begin by kneading the muscles around the hips with your finger tips in gentle , circular motion. Gradually work your way around the surrounding muscles. There is an entire science of pet physical therapy which you can explore.
One of the most helpful forms of therapy for your pet is hydrotherapy and underwater treadmills using the beneficial effects of water to minimize the pain and debility of hip dysplasia. This form of treatment is quite effective in reducing swelling and pain.
Consult your local veterinarian who knows the limitations of your pet before starting a physical therapy program. Rely on the advice or assistance of someone who understands these techniques and their limitations and benefits.

Offering a good (brace) support for hip dysplasia dogs is very important to prevent further injuries. A good brace can afford further stability and support which will aid in decreasing pain and inflammation for active dogs. It is especially useful for senior dogs who are arthritic or injured or recovering pets. It is also extremely useful for younger dogs prone to developing hip dysplasia or joint problems. Selecting a high quality mesh material and combat grade webbing is important so that they can be used often by your pet in any environment.
Initial symptoms that your dog may exhibit can be reduced exercise tolerance, problems going up and down stairs, difficulty rising and lameness after exercise. If your primary care vet or orthopaedic clinician should refer your dog to our rehabilitation service a full physiotherapy assessment is undertaken by one of our chartered physiotherapists. Findings might be – altered gait pattern, with or without lameness, reduced weight-bearing load on the affected limb, weakness of specific muscles (most commonly the gluteal muscles) pain manifested by intolerance to be touched in the affected area or during certain movements or postures and reduced range of movement (ROM). Your dog may exhibit all of or just a few of these clinical signs.
Rehabilitation aims to address the above findings and to maintain and/or prevent progression of the disease. After physiotherapy assessment is completed, a list of focus points is formed and a rehabilitation treatment plan is implemented.
Aims will include the following
| Timeline | Physiotherapy Aims | Rehabilitation Therapy options |
|---|---|---|
| Week 0 to 2 | Reduce post operative swelling |
|
| Reduce muscular guarding and maintain soft tissue flexibility |
| |
| Allow careful limb loading |
| |
| Week 2 to 4 | Progress limb loading and gait re-education |
|
| Increase muscle mass | Low level exercise program and muscle stimulation | |
| Maintain soft tissue length and flexibility |
| |
| Management at home |
| |
| Week 4 to 6 | Continue as above, include core stability exercises | Progression of home exercise program to challenge balance, body awareness and strength |
| Advice on maintaining controlled exercise when dog feeling better | ||
| Week 6 to 12 | Increase exercise tolerance | Increase exercise level, considering land and water based options. |
| Continue to increase core stability | Home exercise program considering land and water based exercises | |
| Week 12 onwards | Return to full function or establish deficits and advise regarding long term management. | Progress to off lead exercise and previous exercise level if appropriate. |