PHYSIOTHERAPY | REHABILITATION | HYDROTHERAPY
OSTEOARTHRITIS IN DOGS
What is Osteoarthritis in Dogs?
Osteoarthritis, also known as degenerative joint disease (DJD), is defined as the progressive and permanent long-term deterioration of the cartilage surrounding the joints. Arthritis is the medical term for inflammation of the joints, while osteoarthritis is the term referring to a form of chronic joint inflammation caused by deterioration of joint cartilage. Older dogs are at the highest risk.
Osteoarthritis occurs when your dog’s joints begin to deteriorate, usually as the dog gets older. With age, your dog’s body produces less glucosamine, a substance that helps maintain joint and cartilage health. As cartilage deteriorates, your dog’s bones begin to rub together, causing pain and inflammation. With time, bone spurs and thickening of the tissue around the joints can occur.
Osteoarthritis can affect any of the joints in your dog’s body. But many times, it can affect the joints in the hips, elbows, lower back, knees and wrists.
The veterinarians in Singapore have made great advances in veterinary medicine. New diagnostic tests and improved treatments have given veterinarians more power in their pursuit of preventing and treating illnesses in our pets. Improved client education and client willingness to provide better care for their animals has also given rise to more geriatric patients being seen at veterinary hospitals across the country. Age is not a disease but it predisposes our pets to more disease.
Everyday we meet someone who tells me their dog has slowed down or has more trouble getting up and down in the last few years. There are numerous reasons for older animals to slow down with age and one of the most prevalent and common is canine arthritis or canine osteoarthritis.
With proper knowledge coupled with proper rehabilitation and physiotherapy, dogs who have been diagnosed with canine arthritis or canine osteoarthritis have better opportunities of living their lives normally, doing the things they used to do.
References
Darryl L. Millis, MS, DVM, DACVS, DACVSMR, CCRP
Professor of Orthopedic Surgery & Director of Surgical Service
Robin Downing, DVM, MS, DAAPM, DACVSMR, CVPP, CCRP
Diplomate of the American Academy of Pain Management, is a a founder and past-president of the International Veterinary Academy of Pain Management.
Janet B. Van Dyke, DVM
Diplomate American College of Veterinary Sports Medicine and Rehabilitation, CCRT, CEO
Ludovica Dragone, DVM, CCRP
Vice President of VEPRA, Veterinary European of Physical Therapy and Rehabilitation Association.
Andrea L. Henderson, DVM, CCRT, CCRP
Resident, Canine Sports Medicine and Rehabilitation
Steven M.Fox, MS, DVM, MBA, PhD
President Securos. Inc
What causes Osteoarthritis in Dogs and are there certain breeds at risk?
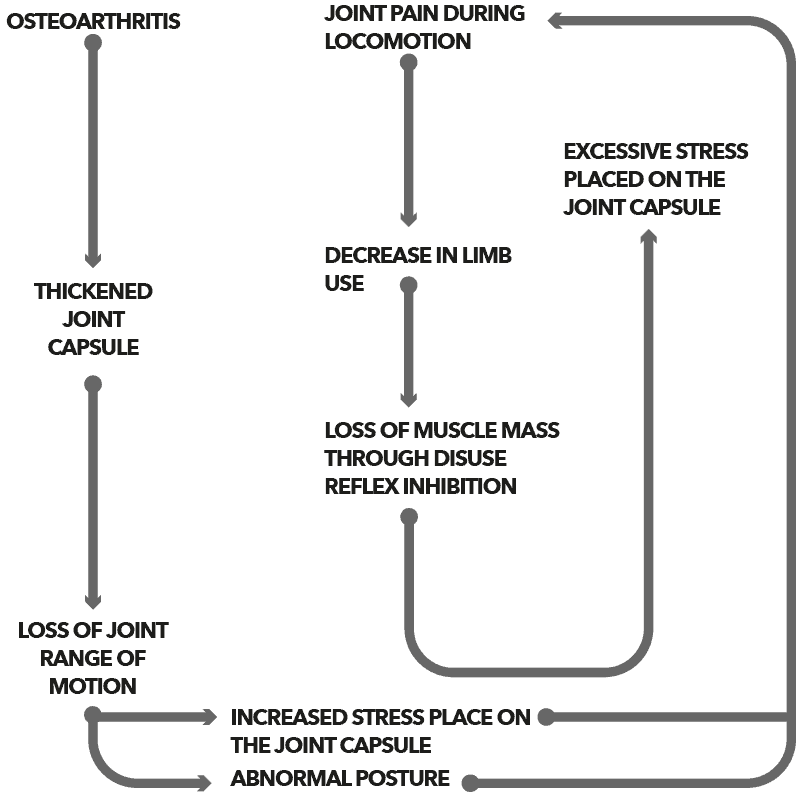
There are then a number of potential TRIGGER factors for osteoarthritis but once triggered, osteoarthritis appears to be a SELF-PERPETUATING PROCESS that generally progresses at a variable rate. So once a patient has it, they have it! Osteoarthritis in dogs is usually triggered by another joint problem such a Hip Dysplasia, Elbow Dysplasia and Osteochodrosis or by trauma to the joint.
Osteoarthritis (OA) is the most common joint disease in dogs. It is reported that one in every five dogs greater than a year old is affected. Incidents increase as dogs age with one in every two dogs ten years or older affected. Given these statistics, our focus on managing osteoarthritis must evolve from simply palliative treatment of well-established disease using just a few modalities to early intervention and a comprehensive multimodal approach.
In the recent years of Singapore, we have seen puppies as young as a 12 months suffering from categories Osteoarthritis (OA), mostly with joint problems caused by congenital defects already present at birth e.g. improperly formed hips (hip dysplasia). This is generally caused by breeders breeding in poor conditions or breeding from bad genes.
Another common category we have seen are degenerative problems influenced by trauma, abnormal wear and tear on joints and cartilage, dislocation, or conditions where bone and cartilage develop abnormally so that flaps of cartilage develop inside the joints.
Many large and giant breed dogs are genetically predisposed to degenerative joint disease and osteoarthritis, especially Golden Retrievers, Labrador Retrievers, German Shepherds, Rottweilers, Great Danes, Doberman Pinschers, Mastiffs, St. Bernards, Huskies and Newfoundlands.
Small dogs can:
- Injure themselves during athletic endeavors, including agility, fly ball, dock diving, among other activities;
- Sustain injuries associated with jumping off beds and couches or tripping on the stairs; and
- Suffer from conditions or genetic diseases that negatively impact joint health. Two such examples in small dogs are: (1) Legg-Calvé-Perthes disease—the spontaneous degeneration of the head of the femur in the hip joint; and (2) poor conformation, which is the alignment of the bones (i.e., the way they are built).

“ Who can resist those sweet puppy eyes and kisses? It is rare for someone to not melt or swoon over a darling furball of energy. But it is rare that someone pauses to ponder over the origin of that puppy. It is not rare that most people are unaware and would be surprised to learn that there is a huge commercial industry dedicated to mass production of these animals“

Signs and Symptoms of Osteoarthritis in Dogs.
Symptoms of Degenerative Joint Diseases (DJD) may vary. Your dog may exhibit a decreased level of activity, occasional lameness, and a stiff gait that worsens with exercise. These symptoms may increase with exercise, long periods of inactivity, or cold weather.
Osteoarthritis can affect one or more joints and can lead to pain, stiffness, joint swelling, lameness and reduced mobility. This can result in a reduced quality of life and prevent dogs from fully participating in everyday activities such as walking, running and swimming.
It is not uncommon for owners to misinterpret these signs as a slowing down due to inevitable old age. It is important to observe dogs closely for the signs of osteoarthritis, including:
- Decreased activity
- Reluctance to walk, run, climb stairs, jump or play
- Stiffness (worse after rest)Limping
- Difficulty rising from a resting position
- Lagging behind on walks
- Soreness when touched
- Yelping or whimpering in pain
- Acting aggressively or withdrawn
- Exhibiting other character changes
Progression of Osteoarthritis in Pets
There is no known cause for primary DJD. However, there are a wide variety of causes for secondary DJD, such as trauma, abnormal wear on joints and cartilage, or a congenital defect present at birth such as an improperly formed hip (also known as hip dysplasia).
Causes of secondary DJD in dogs may include abnormal development of the hip or elbow (hip or elbow dysplasia), dislocation of the kneecap or shoulder, and osteochondritis dissecans (OCD), a condition in which the bone and cartilage develop abnormally so that a flap of cartilage develops within the joint.
Obesity is another factor for DJD, as it increases stress on joints. In addition, dogs with disorders such as diabetes, prolonged steroid treatment, and hyperlaxity (an excessive looseness of the joints) may also be at higher risk for DJD.
The Importance of Pain Management
Dealing with pain is a significant challenge for you as the owner of companion animals and the provider of their medical care. Managing pain goes far beyond the administration of medications. It includes developing a strategy that will increase patient strength and fitness, optimize the pet’s body weight, implement a home exercise program, make appropriate use of safe and effective ambulation assistance devices, and optimize the home environment. However, to allow an effective rehabilitation program to be implemented and to achieve optimum results, logical, safe, and effective use of analgesics is required. This therapy must be tailored to the individual animal, should be multimodal, and needs constant re-evaluation for efficacy and toxicity. This is one of the many reasons why we DO NOT work independently but insist on working with your vets.
Drug and non-drug options should be used in designing a comprehensive management plan in patients with chronic pain associated with osteoarthritis (OA). Non-drug options include cold therapy, heat therapy, massage, stretching, electrical stimulation, therapeutic exercises, and others. Weight management and nutritional strategies used to manage osteoarthritis are reviewed. Ambulation assisting devices and environment modification for osteoarthritic patients should be considered. For most aspects of rehabilitation, such as therapeutic exercise, effective analgesia is required. Drug options include nonsteroidal antiinflammatory drugs, or NSAIDs (COX-1 sparing, coxibs, and dual inhibitors), acetaminophen, N-methyl-D-aspartate (NMDA) antagonists (amantadine), anticonvulsants (gabapentin), and mixed analgesics (tramadol). The logical and safe use of such drugs should be discussed with your vet. Usage of supplements should not contraindicate the efforts of your vets.
” Managing pain includes developing a strategy that will increase patient strength and fitness, optimize the pet’s body weight, implement a home exercise program, making appropriate use of safe and effective ambulation assistance devices, and optimize the home environment. “
Osteoarthritis – The importance of a proper diagnosis process
A diagnosis of DJD may be done based on an assessment of historical symptoms, such as decreased activity or stiffness, as well as a physical examination which will reveal a decreased range of motion, stiff-legged gait, deformity of the joints, and swelling or pain in the joints. Dogs show pain when affected joints are manipulated, the range of movement may be reduced and there may be some creaking, which may be heard as cracking or clicking sounds. Muscle is lost because the joint is not used normally.
It is important to consult you veterinarian for an examination of your dog, which can indicate if your dog has osteoarthritis. The joint may be enlarged due to an increase in fluid in the joint, or new bone development and/or soft tissue thickening around the joint. X-rays can be taken to confirm the changes in the joint and sometimes it is necessary to take samples of joint fluid to rule out other causes of arthritis.
In older canines, bloodwork and a urine sample will help provide valuable information on the dog’s geriatric baseline health. X-rays are an effective tool for identifying OA. They can show bone changes, narrowing of joint spaces, and other physical changes that are known to be associated with arthritis. Magnetic resonance imaging (MRI) and computed tomography (CT) can help visualize joint incongruity and physical cartilage changes.
The importance of Rehabilitation and Physiotherapy for Dogs with Osteoarthritis
Most of our clients referred by veterinarians are mostly suffering from some form of Osteoarthritis, and this is regardless of the age of the dog. Many dogs diagnosed with osteoarthritis that do not require surgery. These dogs can be effectively managed with rehabilitation. Early intervention and support is vital as is a thorough assessment and implementation of a staged rehabilitation treatment plan.
The goals in OA management are to relieve pain, reduce inflammation, improve joint health, increase limb and core muscle strength, increase joint range of motion, improve quality of life and prevent future joint degeneration. Treating OA is best done by blending traditional and alternative therapies thereby creating a multimodal approach. When developing a plan for your pet the veterinarian and us will select therapies that work together to break the cycle of pain, joint stress, weight gain, reduced activity, and muscle atrophy to help restore your pet’s function and quality of life. For example, if you were to compare OA management to a rowing team you would see that when all of the modalities (rowers) work together, the dog has less pain, better function, and improved quality of life (the boat moves smoothly and in a straight line). If one or more of the modalities (rowers) is skipped (like when a rower stops paddling or starts paddling backwards), the dog starts to feel worse (and the boat starts to spin).
Rehabilitation Aims
In the initial stage following diagnosis of Osteoarthritis the aims of rehabilitation will be to:
- Reduce inflammation
- Reduce pain and spasm
- Maintain soft tissues flexibility
- Improve core strength
- Stimulate sensory input
- Re-train postural responses
These above aims continue and progress with time depending on your dogs progress. Aims will ultimately develop to include the following:
- Further strengthen core stability
- Facilitate effective gait
- Increase exercise tolerance and overall cardiovascular fitness
- Return to normal function
Rehabilitation Options
Many different rehabilitation therapeutic modalities can be employed when rehabilitating a dog undergoing conservative management of Osteoarthritis. Possible options might include – laser, or and cold therapy, massage, range of motion exercises and stretches, muscle stimulation, hydrotherapy, home exercise program and advice to prevent further injury.
The following table is an example of a rehabilitation programme our practitioners may use with your dog:
| Timeline | Physiotherapy Aims | Rehabilitation Therapy options |
|---|---|---|
| Week 0 to 4 | Reduce inflammation |
|
| Reduce muscular guarding |
| |
| Improve core stability |
| |
| Increase strength |
| |
| Increase sensation and awareness of body position |
| |
| Maintain soft tissue length and flexibility |
| |
| Management at home |
| |
| Week 4 to 6 | Continue as above |
|
| ||
| ||
| Week 6 to 12 | Increase exercise tolerance |
|
| Continue to increase core stability |
| |
| Week 12 onwards | Return to full function |
|
